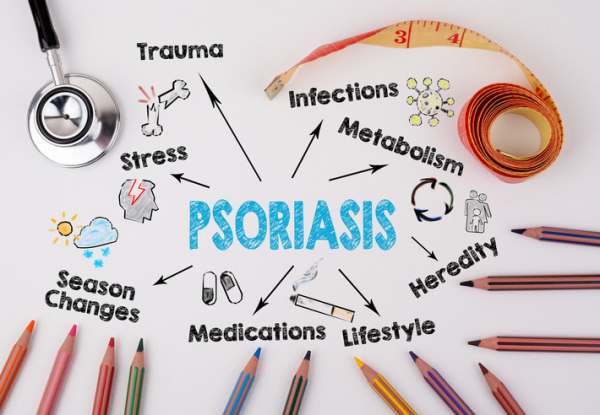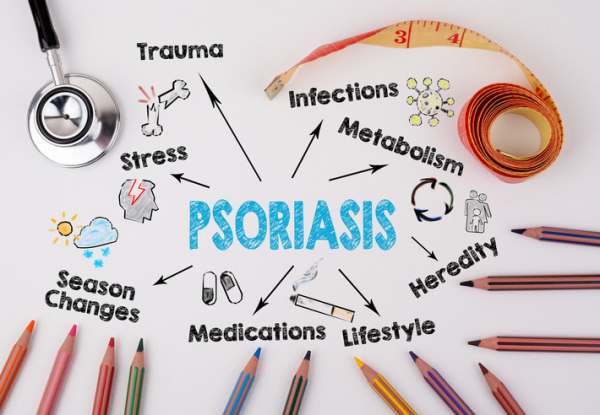
Psoriasis is a chronic disease in which skin cells rapidly divide, causing the skin to develop rough, red, scaly patches. Plaque psoriasis is the most common form: affected skin has sharply defined, inflamed patches (plaques) with silvery or white scales, often near an elbow or on the shins and trunk.
The cause of psoriasis isn’t known, but there are a number of treatment options. Possibly you’ve seen a glossy, happy ad for one of these treatments, a drug called Skyrizi. It’s been in heavy rotation and in 2020, hit number four on a top 10 list for ad spending by a drug company.
Splashing in blue water
A woman in a bathing suit sprints down a dock and jumps into the water with several friends. There’s lots of smiling and splashing. A voiceover says "I have moderate to severe plaque psoriasis. Now, there’s Skyrizi. Three out of four people achieved 90% clearer skin at four months after just two doses."
Then, the voiceover moves to warning mode: "Skyrizi may increase your risk of infections and lower your ability to fight them. Before treatment your doctor should check you for infections and tuberculosis. Tell your doctor if you have an infection or symptoms such as fever, sweats, chills, muscle aches, or cough, or if you plan to or recently received a vaccine."
As these warnings are delivered, we’re treated to uplifting pop music — "nothing is everything," a woman sings — while attractive young people flail about in the water.
"Ask your doctor about Skyrizi," a voice instructs. Did I mention a plane is skywriting the drug’s logo? I guess it’s putting the "sky" in Skyrizi.
What is Skyrizi?
Skyrizi (risankizumab) is an injectable medication that counteracts interleukin-23, a chemical messenger closely involved in the development of psoriasis. The standard dosing is two injections to start, followed a month later by two injections once a month, and then two injections once every three months.
Did you catch that "injectable" part? This is not a pill. If you missed that point while watching the commercial, it’s not your fault. The word "injection" appears once, written in faint letters at the very end of the commercial.
By the way, the FDA has only approved this drug for moderate to severe — not mild — plaque psoriasis. The studies earning approval enrolled people with psoriasis on at least 10% of their skin and two separate measures of severity.
What the ad gets right
- The ad states that 75% of people with moderate to severe psoriasis experienced 90% clearance of their rash within four months after only two doses of Skyrizi. This reflects the findings of research studies (such as this one) that led to the drug’s approval.
- The recommendations regarding screening for infections (including tuberculosis) and telling your doctor if you’ve gotten a recent vaccine are appropriate and should be standard practice. By lowering the ability to fight infection, this drug can make current infections worse. It may reduce the benefit of certain vaccines, or increase the risk of infection when a person gets a certain type of vaccine called a live-attenuated vaccine.
And the theme song? People with visible psoriasis often cover up their skin due to embarrassment or stigma. The rash isn’t a contagious infection or a reflection of poor health, but other people may react as if it is. So, an effective treatment could potentially allow some to forego covering up and show more skin: it means "everything" to someone suffering with psoriasis to cover "nothing." Thus, a theme song is born.
What else do you need to know?
A few things about this ad may be confusing or incomplete, including:
- Currently, each dose of Skyrizi is actually two injections. So, a more accurate way to summarize its effectiveness would be to say that improvement occurred within four months after four injections (rather than "just two doses").
- Like most newer injectable medications, this one is quite expensive: a year's supply could cost nearly $70,000. The drug maker offers a patient assistance program for people with low income or limited health insurance, but not everyone qualifies. Health insurance plans generally require justification from your doctor for medications like Skyrizi, and your insurer may decide not to cover it. Even if covered, this prior approval process can delay starting the medication, which may still be expensive due to copays and/or deductibles.
- There is no mention of the many other options to treat psoriasis, some of which are far less costly. These include medications that do not have to be injected (such as oral methotrexate or apremilast), and UV light therapy (phototherapy). And there are other injectable medications. So, ask your doctor about the best options for you.
The bottom line
Some people appreciate the information provided by medication ads. Others favor a ban on such advertising, as is the case in most other countries. And recently, two advocacy groups asked the FDA not to allow drug ads to play music when the risks of drug side effects are presented, arguing that it distracts consumers from focusing on this important information.
Since these ads probably are not going away anytime soon, keep in mind that they may spin information in a positive light and leave out other important information altogether. So, be skeptical and ask questions. Get your medication information from your doctor or another unbiased, authoritative source, not a company selling a product.
Regardless of how you feel about medical advertising, it’s hard to hate the Skyrizi theme song. Feel free to sing along.